Many people wonder how Justice Ruth Bader Ginsburg and my father, the late Justice Antonin Scalia, managed to be such good friends despite holding such different ideological views.

— FOX News: Christopher Scalia

Many people wonder how Justice Ruth Bader Ginsburg and my father, the late Justice Antonin Scalia, managed to be such good friends despite holding such different ideological views.

— FOX News: Christopher Scalia

The US wild pig population is soaring and rapidly multiplying, which experts believe is a ticking ‘feral swine bomb,’ according to a report on Saturday.

— FOX News: David Aaro

The late Justice grew up in Midwood neighborhood, Brooklyn, N.Y.C., formed by its schools, library and synagogue. She was remembered across the borough and city.

— NYT: Troy Closson


— FOX News

Brett Favre showed his support for Tom Brady on Sunday as the Tampa Bay Buccaneers were getting set to play the Carolina Panthers in the quarterback’s home debut.

— FOX News: Ryan Gaydos

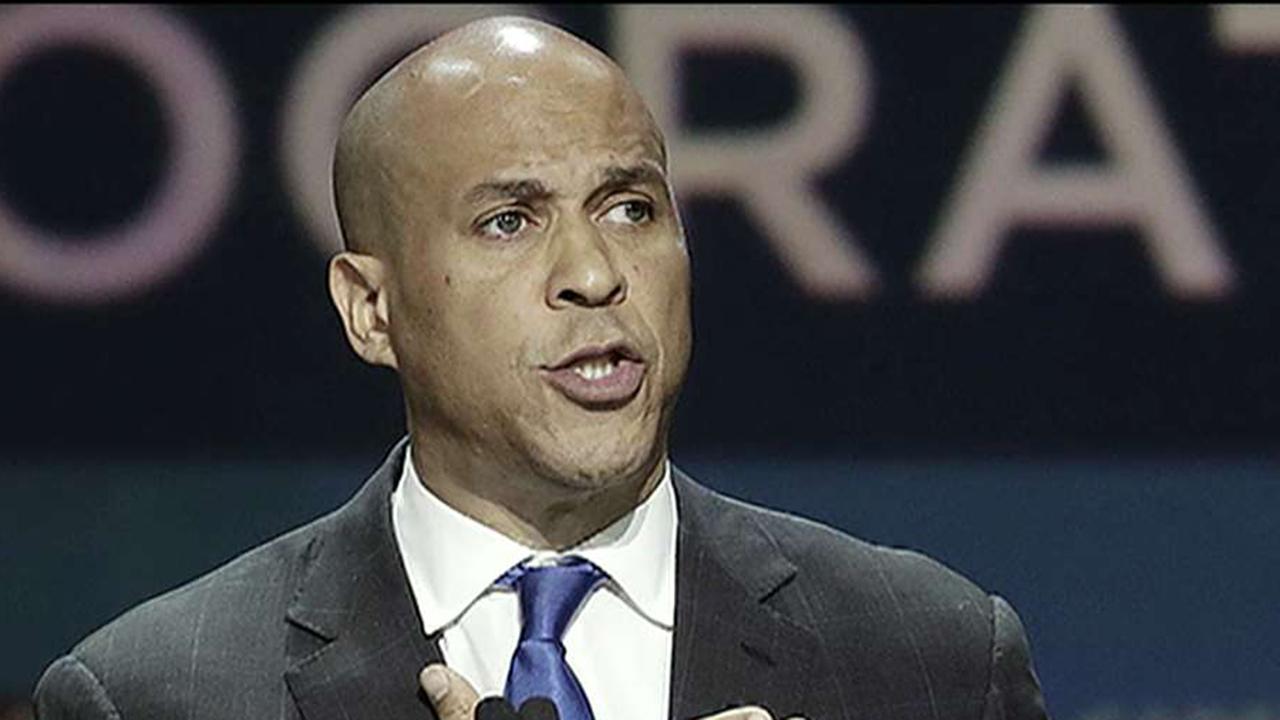
Senate Judiciary Committee member Cory Booker, D-N.J., warned Republicans would harm the Supreme Court’s legitimacy by forcing through a nominee.
— FOX News: Tyler Olson
LYNPARZA is the Only PARP Inhibitor to Demonstrate Improved Overall Survival in Metastatic Castration-Resistant Prostate Cancer
KENILWORTH, N.J.–(BUSINESS WIRE)–$MRK #MRK–AstraZeneca and Merck (NYSE: MRK), known as MSD outside the United States and Canada, today announced final results from the Phase 3 PROfound trial which showed LYNPARZA demonstrated a statistically significant and clinically meaningful improvement in overall survival (OS) versus enzalutamide or abiraterone in men with metastatic castration-resistant prostate cancer (mCRPC) who have BRCA1/2 or ATM gene mutations. Patients had progressed on prior treatment with enzalutamide and/or abiraterone.
Prostate cancer is the second most common type of cancer in men, with an estimated 1.3 million new patients diagnosed worldwide in 2018. Approximately 20-30% of men with mCRPC have an homologous recombination repair (HRR) gene mutation, of which BRCA1/2 and ATM mutations are a subpopulation. Approximately 10-20% of early stage hormone-sensitive prostate cancer cases will develop into CRPC within approximately five years.
In the key secondary endpoint of OS in men with BRCA1/2 or ATM gene mutations, LYNPARZA reduced the risk of death by 31% vs. retreatment with enzalutamide or abiraterone (HR 0.69 [95% CI, 0.50, 0.97], p=0.0175). Median OS was 19.1 months for LYNPARZA vs. 14.7 months for enzalutamide or abiraterone, despite 66% of men on these treatments having crossed over to receive treatment with LYNPARZA following disease progression.
An exploratory analysis also showed a non-statistically significant improvement in OS in the overall trial population of men with HRR gene mutations (BRCA1/2, ATM, CDK12 and 11 other HRR-mutated [HRRm] genes), reducing the risk of death by 21% with LYNPARZA vs. enzalutamide or abiraterone (HR 0.79 [95% CI, 0.61, 1.03]. Median OS was 17.3 months vs. 14 months for enzalutamide or abiraterone.
The most common adverse reactions (ARs) ≥15% were anemia (50%), nausea (43%), fatigue/asthenia (42%), decreased appetite (31%), diarrhea (21%), vomiting (20%) and constipation (19%). Grade 3 or above ARs were anemia (23%), nausea (2%), fatigue or asthenia (3%), decreased appetite (2%) and diarrhea (1%). Twenty percent of patients on LYNPARZA discontinued treatment due to ARs and 23% had their dose reduced due to an AR.
Dr. Johann de Bono, one of the principal investigators of the PROfound trial and head of drug development at the Institute for Cancer Research and the Royal Marsden Hospital, said, “LYNPARZA has demonstrated significant clinical benefit across key endpoints in PROfound and the final overall survival results for men with BRCA1/2 or ATM mutations reinforce its potential to change the standard of care for men with metastatic castration-resistant prostate cancer. The PROfound trial shows that LYNPARZA can play an important role in this new era of precision medicine in prostate cancer, bringing targeted therapy at a molecular level to patients with a historically poor prognosis and few treatment options.”
Dr. José Baselga, executive vice president, Oncology R&D, AstraZeneca said, “These results help to transform the treatment landscape in certain men with metastatic castration-resistant prostate cancer, where overall survival has been very difficult to achieve. LYNPARZA is the only PARP inhibitor to demonstrate overall survival versus enzalutamide or abiraterone for men with BRCA or ATM mutations. We look forward to continuing to bring LYNPARZA to these patients around the world.”
Dr. Roy Baynes, senior vice president and head of global clinical development, chief medical officer, Merck Research Laboratories, said, “The PROfound trial is the first positive Phase 3 trial using molecular biomarker testing to help identify treatment options for certain men with metastatic castration resistant prostate cancer. These results further underpin the importance of genomic testing for HRR gene mutations to help identify this at-risk patient population and help physicians make treatment decisions. These results demonstrate the potential of LYNPARZA for mCRPC patients with certain HRR mutations.”
Final OS results from the PROfound trial were presented on Sunday, Sept. 20, 2020, during the Presidential Symposium at the European Society for Medical Oncology (ESMO) Virtual Congress 2020 and published simultaneously in The New England Journal of Medicine.
Summary of OS results
OS data cut-off date was March 20, 2020.
|
|
Men with BRCA1/2 and ATM Secondary Endpoint |
Overall population of men with HRR mutations (Cohorts A+B) Exploratory Endpoint |
||
|
LYNPARZA n=162 |
Control n=83 |
LYNPARZA n=256 |
Control n=131 |
|
|
Median, months |
19.1 |
14.7
|
17.3 |
14.0
|
|
Hazard ratio (95% CI)
|
0.69 (0.50, 0.97)
|
0.79 (0.61, 1.03)
|
||
|
P-value |
0.0175 |
N/A |
||
The Phase 3 PROfound trial had met its primary endpoint in August 2019, showing significantly improved radiographic progression-free survival (rPFS) in men with mutations in BRCA1/2 or ATM genes, and had met a key secondary endpoint of rPFS in the overall HRRm population, which formed the basis of the U.S. Food and Drug Administration approval in May 2020. Regulatory reviews are ongoing in the EU and other regions.
AstraZeneca and Merck are exploring additional trials in metastatic prostate cancer including the ongoing Phase 3 PROpel trial, with first data expected in 2021, evaluating LYNPARZA as a first-line medicine for patients with mCRPC in combination with abiraterone acetate versus abiraterone acetate alone.
About PROfound
PROfound is a prospective, multi-center, randomized, open-label, Phase 3 trial evaluating the efficacy and safety of LYNPARZA versus enzalutamide or abiraterone in patients with mCRPC who have progressed on prior treatment with abiraterone or enzalutamide and have a qualifying HRR tumor mutation (BRCA1/2, ATM, CDK12, BARD1, BRIP2, CHEK1, CHEK2, PALB2, PPP2R2A, RAD51B, RAD51D, RAD54L).
The trial was designed to analyze patients with HRRm genes in two cohorts: the primary endpoint was rPFS in those with mutations in BRCA1/2 or ATM genes and then, if LYNPARZA showed clinical benefit, a formal analysis was performed of the overall trial population of patients with HRRm genes (BRCA1/2, ATM, CDK12 and 11 other HRR mutated genes; a key secondary endpoint).
In the U.S., patients are selected for treatment with LYNPARZA based on the following FDA-approved companion diagnostics:
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS
There are no contraindications for LYNPARZA.
WARNINGS AND PRECAUTIONS
Myelodysplastic Syndrome/Acute Myeloid Leukemia (MDS/AML): Occurred in <1.5% of patients exposed to LYNPARZA monotherapy, and the majority of events had a fatal outcome. The duration of therapy in patients who developed secondary MDS/AML varied from <6 months to >2 years. All of these patients had previous chemotherapy with platinum agents and/or other DNA-damaging agents, including radiotherapy, and some also had a history of more than one primary malignancy or of bone marrow dysplasia.
Do not start LYNPARZA until patients have recovered from hematological toxicity caused by previous chemotherapy (≤Grade 1). Monitor complete blood count for cytopenia at baseline and monthly thereafter for clinically significant changes during treatment. For prolonged hematological toxicities, interrupt LYNPARZA and monitor blood count weekly until recovery.
If the levels have not recovered to Grade 1 or less after 4 weeks, refer the patient to a hematologist for further investigations, including bone marrow analysis and blood sample for cytogenetics. Discontinue LYNPARZA if MDS/AML is confirmed.
Pneumonitis: Occurred in <1% of patients exposed to LYNPARZA, and some cases were fatal. If patients present with new or worsening respiratory symptoms such as dyspnea, cough, and fever, or a radiological abnormality occurs, interrupt LYNPARZA treatment and initiate prompt investigation. Discontinue LYNPARZA if pneumonitis is confirmed and treat patient appropriately.
Embryo-Fetal Toxicity: Based on its mechanism of action and findings in animals, LYNPARZA can cause fetal harm. A pregnancy test is recommended for females of reproductive potential prior to initiating treatment.
Females
Advise females of reproductive potential of the potential risk to a fetus and to use effective contraception during treatment and for 6 months following the last dose.
Males
Advise male patients with female partners of reproductive potential or who are pregnant to use effective contraception during treatment and for 3 months following the last dose of LYNPARZA and to not donate sperm during this time.
Venous Thromboembolic Events: Including pulmonary embolism, occurred in 7% of patients with metastatic castration-resistant prostate cancer who received LYNPARZA plus androgen deprivation therapy (ADT) compared to 3.1% of patients receiving enzalutamide or abiraterone plus ADT in the PROfound study. Patients receiving LYNPARZA and ADT had a 6% incidence of pulmonary embolism compared to 0.8% of patients treated with ADT plus either enzalutamide or abiraterone. Monitor patients for signs and symptoms of venous thrombosis and pulmonary embolism, and treat as medically appropriate, which may include long-term anticoagulation as clinically indicated.
ADVERSE REACTIONS—First-Line Maintenance BRCAm Advanced Ovarian Cancer
Most common adverse reactions (Grades 1-4) in ≥10% of patients in clinical trials of LYNPARZA in the first-line maintenance setting for SOLO-1 were: nausea (77%), fatigue (67%), abdominal pain (45%), vomiting (40%), anemia (38%), diarrhea (37%), constipation (28%), upper respiratory tract infection/influenza/ nasopharyngitis/bronchitis (28%), dysgeusia (26%), decreased appetite (20%), dizziness (20%), neutropenia (17%), dyspepsia (17%), dyspnea (15%), leukopenia (13%), UTI (13%), thrombocytopenia (11%), and stomatitis (11%).
Most common laboratory abnormalities (Grades 1-4) in ≥25% of patients in clinical trials of LYNPARZA in the first-line maintenance setting for SOLO-1 were: decrease in hemoglobin (87%), increase in mean corpuscular volume (87%), decrease in leukocytes (70%), decrease in lymphocytes (67%), decrease in absolute neutrophil count (51%), decrease in platelets (35%), and increase in serum creatinine (34%).
ADVERSE REACTIONS—First-Line Maintenance Advanced Ovarian Cancer in Combination with Bevacizumab
Most common adverse reactions (Grades 1-4) in ≥10% of patients treated with LYNPARZA/bevacizumab compared to a ≥5% frequency for placebo/bevacizumab in the first-line maintenance setting for PAOLA-1 were: nausea (53%), fatigue (including asthenia) (53%), anemia (41%), lymphopenia (24%), vomiting (22%) and leukopenia (18%). In addition, the most common adverse reactions (≥10%) for patients receiving LYNPARZA/bevacizumab irrespective of the frequency compared with the placebo/bevacizumab arm were: diarrhea (18%), neutropenia (18%), urinary tract infection (15%), and headache (14%).
In addition, venous thromboembolic events occurred more commonly in patients receiving LYNPARZA/bevacizumab (5%) than in those receiving placebo/bevacizumab (1.9%).
Most common laboratory abnormalities (Grades 1-4) in ≥25% of patients for LYNPARZA in combination with bevacizumab in the first-line maintenance setting for PAOLA-1 were: decrease in hemoglobin (79%), decrease in lymphocytes (63%), increase in serum creatinine (61%), decrease in leukocytes (59%), decrease in absolute neutrophil count (35%), and decrease in platelets (35%).
ADVERSE REACTIONS—Maintenance Recurrent Ovarian Cancer
Most common adverse reactions (Grades 1-4) in ≥20% of patients in clinical trials of LYNPARZA in the maintenance setting for SOLO-2 were: nausea (76%), fatigue (including asthenia) (66%), anemia (44%), vomiting (37%), nasopharyngitis/upper respiratory tract infection (URI)/influenza (36%), diarrhea (33%), arthralgia/myalgia (30%), dysgeusia (27%), headache (26%), decreased appetite (22%), and stomatitis (20%).
Study 19: nausea (71%), fatigue (including asthenia) (63%), vomiting (35%), diarrhea (28%), anemia (23%), respiratory tract infection (22%), constipation (22%), headache (21%), decreased appetite (21%), and dyspepsia (20%).
Most common laboratory abnormalities (Grades 1-4) in ≥25% of patients in clinical trials of LYNPARZA in the maintenance setting (SOLO-2/Study 19) were: increase in mean corpuscular volume (89%/82%), decrease in hemoglobin (83%/82%), decrease in leukocytes (69%/58%), decrease in lymphocytes (67%/52%), decrease in absolute neutrophil count (51%/47%), increase in serum creatinine (44%/45%), and decrease in platelets (42%/36%).
ADVERSE REACTIONS—Advanced gBRCAm Ovarian Cancer
Most common adverse reactions (Grades 1-4) in ≥20% of patients in clinical trials of LYNPARZA for advanced gBRCAm ovarian cancer after 3 or more lines of chemotherapy (pooled from 6 studies) were: fatigue/asthenia (66%), nausea (64%), vomiting (43%), anemia (34%), diarrhea (31%), nasopharyngitis/upper respiratory tract infection (URI) (26%), dyspepsia (25%), myalgia (22%), decreased appetite (22%), and arthralgia/musculoskeletal pain (21%).
Most common laboratory abnormalities (Grades 1-4) in ≥25% of patients in clinical trials of LYNPARZA for advanced gBRCAm ovarian cancer (pooled from 6 studies) were: decrease in hemoglobin (90%), mean corpuscular volume elevation (57%), decrease in lymphocytes (56%), increase in serum creatinine (30%), decrease in platelets (30%), and decrease in absolute neutrophil count (25%).
ADVERSE REACTIONS—gBRCAm, HER2-negative Metastatic Breast Cancer
Most common adverse reactions (Grades 1-4) in ≥20% of patients in OlympiAD were: nausea (58%), anemia (40%), fatigue (including asthenia) (37%), vomiting (30%), neutropenia (27%), respiratory tract infection (27%), leukopenia (25%), diarrhea (21%), and headache (20%).
Most common laboratory abnormalities (Grades 1-4) in >25% of patients in OlympiAD were: decrease in hemoglobin (82%), decrease in lymphocytes (73%), decrease in leukocytes (71%), increase in mean corpuscular volume (71%), decrease in absolute neutrophil count (46%), and decrease in platelets (33%).
ADVERSE REACTIONS—First-Line Maintenance gBRCAm Metastatic Pancreatic Adenocarcinoma
Most common adverse reactions (Grades 1-4) in ≥10% of patients in clinical trials of LYNPARZA in the first-line maintenance setting for POLO were: fatigue (60%), nausea (45%), abdominal pain (34%), diarrhea (29%), anemia (27%), decreased appetite (25%), constipation (23%), vomiting (20%), back pain (19%), arthralgia (15%), rash (15%), thrombocytopenia (14%), dyspnea (13%), neutropenia (12%), nasopharyngitis (12%), dysgeusia (11%), and stomatitis (10%).
Most common laboratory abnormalities (Grades 1-4) in ≥25% of patients in clinical trials of LYNPARZA in the first-line maintenance setting for POLO were: increase in serum creatinine (99%), decrease in hemoglobin (86%), increase in mean corpuscular volume (71%), decrease in lymphocytes (61%), decrease in platelets (56%), decrease in leukocytes (50%), and decrease in absolute neutrophil count (25%).
ADVERSE REACTIONS—HRR Gene-mutated Metastatic Castration Resistant Prostate Cancer
Most common adverse reactions (Grades 1-4) in ≥10% of patients in clinical trials of LYNPARZA for PROfound were: anemia (46%), fatigue (including asthenia) (41%), nausea (41%), decreased appetite (30%), diarrhea (21%), vomiting (18%), thrombocytopenia (12%), cough (11%), and dyspnea (10%).
Most common laboratory abnormalities (Grades 1-4) in ≥25% of patients in clinical trials of LYNPARZA for PROfound were: decrease in hemoglobin (98%), decrease in lymphocytes (62%), decrease in leukocytes (53%), and decrease in absolute neutrophil count (34%).
DRUG INTERACTIONS
Anticancer Agents: Clinical studies of LYNPARZA with other myelosuppressive anticancer agents, including DNA-damaging agents, indicate a potentiation and prolongation of myelosuppressive toxicity.
CYP3A Inhibitors: Avoid coadministration of strong or moderate CYP3A inhibitors when using LYNPARZA. If a strong or moderate CYP3A inhibitor must be coadministered, reduce the dose of LYNPARZA. Advise patients to avoid grapefruit, grapefruit juice, Seville oranges, and Seville orange juice during LYNPARZA treatment.
CYP3A Inducers: Avoid coadministration of strong or moderate CYP3A inducers when using LYNPARZA.
USE IN SPECIFIC POPULATIONS
Lactation: No data are available regarding the presence of olaparib in human milk, its effects on the breastfed infant or on milk production. Because of the potential for serious adverse reactions in the breastfed infant, advise a lactating woman not to breastfeed during treatment with LYNPARZA and for 1 month after receiving the final dose.
Pediatric Use: The safety and efficacy of LYNPARZA have not been established in pediatric patients.
Hepatic Impairment: No adjustment to the starting dose is required in patients with mild or moderate hepatic impairment (Child-Pugh classification A and B). There are no data in patients with severe hepatic impairment (Child-Pugh classification C).
Renal Impairment: No dosage modification is recommended in patients with mild renal impairment (CLcr 51-80 mL/min estimated by Cockcroft-Gault). In patients with moderate renal impairment (CLcr 31-50 mL/min), reduce the dose of LYNPARZA to 200 mg twice daily. There are no data in patients with severe renal impairment or end-stage renal disease (CLcr ≤30 mL/min).
INDICATIONS
LYNPARZA is a poly (ADP-ribose) polymerase (PARP) inhibitor indicated:
First-Line Maintenance BRCAm Advanced Ovarian Cancer
For the maintenance treatment of adult patients with deleterious or suspected deleterious germline or somatic BRCA-mutated (gBRCAm or sBRCAm) advanced epithelial ovarian, fallopian tube or primary peritoneal cancer who are in complete or partial response to first-line platinum-based chemotherapy. Select patients for therapy based on an FDA-approved companion diagnostic for LYNPARZA.
First-Line Maintenance HRD Positive Advanced Ovarian Cancer in Combination with Bevacizumab
In combination with bevacizumab for the maintenance treatment of adult patients with advanced epithelial ovarian, fallopian tube or primary peritoneal cancer who are in complete or partial response to first-line platinum-based chemotherapy and whose cancer is associated with homologous recombination deficiency (HRD) positive status defined by either:
Select patients for therapy based on an FDA-approved companion diagnostic for LYNPARZA.
Maintenance Recurrent Ovarian Cancer
For the maintenance treatment of adult patients with recurrent epithelial ovarian, fallopian tube or primary peritoneal cancer, who are in complete or partial response to platinum-based chemotherapy.
Advanced gBRCAm Ovarian Cancer
For the treatment of adult patients with deleterious or suspected deleterious germline BRCA-mutated (gBRCAm) advanced ovarian cancer who have been treated with 3 or more prior lines of chemotherapy. Select patients for therapy based on an FDA-approved companion diagnostic for LYNPARZA.
gBRCAm HER2-negative Metastatic Breast Cancer
For the treatment of adult patients with deleterious or suspected deleterious gBRCAm, human epidermal growth factor receptor 2 (HER2)-negative metastatic breast cancer, who have been treated with chemotherapy in the neoadjuvant, adjuvant or metastatic setting. Patients with hormone receptor (HR)-positive breast cancer should have been treated with a prior endocrine therapy or be considered inappropriate for endocrine therapy. Select patients for therapy based on an FDA-approved companion diagnostic for LYNPARZA.
First-Line Maintenance gBRCAm Metastatic Pancreatic Cancer
For the maintenance treatment of adult patients with deleterious or suspected deleterious gBRCAm metastatic pancreatic adenocarcinoma whose disease has not progressed on at least 16 weeks of a first-line platinum-based chemotherapy regimen. Select patients for therapy based on an FDA-approved companion diagnostic for LYNPARZA.
HRR Gene-mutated Metastatic Castration Resistant Prostate Cancer
For the treatment of adult patients with deleterious or suspected deleterious germline or somatic homologous recombination repair (HRR) gene-mutated metastatic castration-resistant prostate cancer (mCRPC) who have progressed following prior treatment with enzalutamide or abiraterone. Select patients for therapy based on an FDA-approved companion diagnostic for LYNPARZA.
Please click here for complete Prescribing Information, including Patient Information (Medication Guide).
About LYNPARZA® (olaparib)
LYNPARZA is a first-in-class PARP inhibitor and the first targeted treatment to potentially exploit DNA damage response (DDR) pathway deficiencies, such as BRCA mutations, to preferentially kill cancer cells. Inhibition of PARP with LYNPARZA leads to the trapping of PARP bound to DNA single-strand breaks, stalling of replication forks, their collapse and the generation of DNA double-strand breaks and cancer cell death. LYNPARZA is being tested in a range of tumor types with defects and dependencies in the DDR.
LYNPARZA, which is being jointly developed and commercialized by AstraZeneca and Merck, has a broad and advanced clinical trial development program, and AstraZeneca and Merck are working together to understand how it may affect multiple PARP-dependent tumors as a monotherapy and in combination across multiple cancer types.
About Metastatic Castration-Resistant Prostate Cancer (mCRPC)
Prostate cancer is the second-most common cancer in men, with an estimated 1.3 million new cases diagnosed worldwide in 2018, and is associated with a significant mortality rate. Development of prostate cancer is often driven by male sex hormones called androgens, including testosterone. In patients with mCRPC, their prostate cancer grows and spreads to other parts of the body despite the use of androgen-deprivation therapy to block the action of male sex hormones. Approximately 10-20% of men with advanced prostate cancer will develop CRPC within five years, and at least 84% of these men will have metastases at the time of CRPC diagnosis. Of men with no metastases at CRPC diagnosis, 33% are likely to develop metastases within two years. Despite advances in treatment for men with mCRPC, five-year survival is low and extending survival remains a key goal for treating these men.
About Homologous Recombination Repair (HRR) Mutations
HRR mutations occur in approximately 20-30% of patients with mCRPC. HRR genes allow for accurate repair of damaged DNA in normal cells. HRR deficiency (HRD) means the DNA damage cannot be repaired, and can result in normal cell death. This is different in cancer cells, where a mutation in HRR pathways leads to abnormal cell growth and therefore cancer. HRD is a well-documented target for PARP inhibitors, such as LYNPARZA.
Contacts
Media:
Pamela Eisele
(267) 305-3558
Steve Wanczyk
(267) 305-5563
Investor:
Peter Dannenbaum
(908) 740-1037
Courtney Ronaldo
(908) 740-6132
Researchers Share New Data for Vibostolimab (MK-7684), Merck’s Anti-TIGIT Therapy, as Monotherapy and in Combination With KEYTRUDA® (pembrolizumab); First-Time Results for First-in-Class MK-4830 (Anti-ILT4 Therapy); and Late-Breaking Data for MK-6482 (HIF-2α Inhibitor)
Merck to Initiate Phase 3 Study of Vibostolimab in Non-Small Cell Lung Cancer in First Half of 2021
KENILWORTH, N.J.–(BUSINESS WIRE)–$MRK #MRK–Merck (NYSE: MRK), known as MSD outside the United States and Canada, today announced the presentation of new data for three investigational medicines in Merck’s diverse and expansive oncology pipeline: vibostolimab (MK-7684), an anti-TIGIT therapy; MK-4830, a first-in-class anti-ILT4 therapy; and MK-6482, an oral HIF-2α inhibitor. Data from cohort expansions of a Phase 1b trial evaluating vibostolimab, as monotherapy and in combination with KEYTRUDA, Merck’s anti-PD-1 therapy, in patients with metastatic non-small cell lung cancer (NSCLC; Abstract #1410P and Abstract #1400P), and first-time Phase 1 data for MK-4830 in patients with advanced solid tumors (Abstract #524O), demonstrated acceptable safety profiles for these two investigational medicines and early signals of anti-tumor activity. Additionally, late-breaking Phase 2 data for MK-6482 showed anti-tumor responses in von Hippel-Lindau (VHL) disease patients with clear cell renal cell carcinoma (RCC) and other tumors (Abstract #LBA26).
“The new data for these three investigational medicines are encouraging and highlight continued momentum in our rapidly expanding oncology pipeline,” Dr. Eric H. Rubin, senior vice president, early-stage development, clinical oncology, Merck Research Laboratories. “Over the past five years, KEYTRUDA has become foundational in the treatment of certain advanced cancers. Our broad oncology portfolio and promising pipeline candidates are a testament to our commitment to bring forward innovative new medicines to address unmet medical needs in cancer care.”
Vibostolimab (Anti-TIGIT Therapy): Early Findings in Metastatic NSCLC (Abstract #1410P and Abstract #1400P)
Vibostolimab in combination with KEYTRUDA was evaluated in patients with metastatic NSCLC who had not previously received anti–PD-1/PD-L1 therapy, but the majority of whom had received >1 prior lines of therapy (73%, n=30/41) in Abstract #1410P. In Part B of the first-in-human, open-label, Phase 1 trial (NCT02964013) all patients received vibostolimab (200 or 210 mg) in combination with KEYTRUDA (200 mg) on Day 1 of each three-week cycle for up to 35 cycles. The primary endpoints of the study were safety and tolerability. Secondary endpoints included objective response rate (ORR), duration of response (DOR) and progression-free survival (PFS) based on investigator review per RECIST v1.1. In this anti-PD-1/PD-L1 naïve study, vibostolimab in combination with KEYTRUDA had a manageable safety profile and demonstrated promising anti-tumor activity. Treatment-related adverse events (TRAEs) with vibostolimab in combination with KEYTRUDA occurred in 34 patients (83%). The most frequent TRAEs (≥20%) were pruritus (34%), hypoalbuminemia (29%) and pyrexia (20%). Grade 3-5 TRAEs occurred in six patients (15%). No deaths due to TRAEs occurred. Across all patients enrolled, treatment with vibostolimab in combination with KEYTRUDA demonstrated an ORR of 29% (95% CI, 16-46) and median PFS was 5.4 months (95% CI, 2.1-8.2). The median DOR was not reached (range, 4 to 17+ months). Among patients whose tumors express PD-L1 (tumor proportion score [TPS] ≥1%) (n=13), the ORR was 46% (95% CI, 19-75) and median PFS was 8.4 months (95% CI, 3.9-10.2). Among patients whose tumors express PD-L1 (TPS <1%) (n=12), the ORR was 25% (95% CI, 6-57), and median PFS was 4.1 months (95% CI, 1.9-not reached [NR]). PD-L1 status was not available for 16 patients. Median follow-up for the study was 11 months (range, 7 to 18).
Additional data from a separate cohort of the same Phase 1b trial evaluated vibostolimab as monotherapy (n=41) and in combination with KEYTRUDA (n=38) in patients with metastatic NSCLC whose disease progressed on prior anti-PD-1/PD-L1 therapy (Abstract #1400P). In the study, 78% of patients had received >2 lines of prior therapy. In the study, patients received vibostolimab monotherapy (200 or 210 mg) or vibostolimab (200 or 210 mg) in combination with KEYTRUDA (200 mg) on Day 1 of each three-week cycle for up to 35 cycles. The primary endpoints of the study were safety and tolerability. Secondary endpoints included ORR and DOR. Vibostolimab as monotherapy or in combination with KEYTRUDA had a manageable safety profile and demonstrated modest anti-tumor activity in patients whose disease was refractory to PD-1/PD-L1 inhibition, most of whom had previously received several lines of therapy for advanced disease prior to enrollment. Grade 3-5 TRAEs occurred in 15% of patients receiving vibostolimab monotherapy and 13% of patients receiving vibostolimab in combination with KEYTRUDA. The most common TRAEs (≥10% in either arm) were pruritus, fatigue, rash, arthralgia and decreased appetite. One patient died due to treatment-related pneumonitis in the vibostolimab and KEYTRUDA combination arm. The ORR was 7% (95% CI, 2-20) with vibostolimab monotherapy and 5% (95% CI, <1-18) with vibostolimab in combination with KEYTRUDA. The median DOR was 9 months (range, 9 to 9) with vibostolimab monotherapy and 13 months (range, 4+ to 13) with vibostolimab in combination with KEYTRUDA.
Data from these cohort expansion studies are encouraging and support the continued development of vibostolimab, which is being evaluated alone and in combination with KEYTRUDA across multiple solid tumors, including NSCLC and melanoma. In the ongoing Phase 2 KEYNOTE-U01 umbrella study (NCT04165798), substudy KEYNOTE-01A (NCT04165070) is evaluating vibostolimab in combination with KEYTRUDA plus chemotherapy for the first-line treatment of patients with advanced NSCLC who had not received prior treatment with an anti-PD-1/PD-L1. Merck plans to initiate a Phase 3 study of vibostolimab in NSCLC in the first half of 2021. Ongoing trials in melanoma include the Phase 1/2 KEYNOTE-U02 umbrella study comprised of three substudies evaluating vibostolimab in combination with KEYTRUDA across treatment settings (substudy 02A: NCT04305041, substudy 02B: NCT04305054 and substudy 02C: NCT04303169).
MK-4830 (Anti-ILT4 Therapy): Initial Results in Advanced Solid Tumors (Abstract #524O)
In this first-in-human Phase 1, open-label, multi-arm, multi-center, dose escalation study (NCT03564691), MK-4830, Merck’s first-in-class anti-ILT4 therapy, was evaluated as monotherapy (n=50) and in combination with KEYTRUDA (n=34) in patients with advanced solid tumors. The majority of patients enrolled in the study (51%) had received three or more prior lines of therapy. MK-4830 was administered intravenously at escalating doses every three weeks alone or in combination with KEYTRUDA (200 mg every three weeks). The primary endpoints of the dose escalation part of the study were safety and tolerability; Pharmacokinetics was a secondary endpoint, and exploratory objectives included ORR per RECIST v1.1, evaluation of receptor occupancy and immune correlates of response in blood and tumor.
Findings showed that MK-4830 as monotherapy and in combination with KEYTRUDA had an acceptable safety profile and demonstrated dose-related evidence of target engagement in patients with advanced solid tumors. No dose-limiting toxicities were observed; the maximum-tolerated dose was not reached. Any-grade adverse events were consistent with those associated with KEYTRUDA. Treatment-related AEs occurred in 54% (n=28/52) of patients who received MK-4830 in combination with KEYTRUDA and 48% (n=24/50) of patients who received MK-4830 monotherapy; the majority were Grade 1 and 2. Preliminary efficacy data showed an ORR of 24% (n=8/34) in patients who received MK-4830 in combination with KEYTRUDA. All responses occurred in heavily pretreated patients, including five who had progressed on prior anti-PD-1 therapy (n=5/11). Some patients received more than one year of treatment, and treatment is ongoing in several patients.
These early data support the continued development of MK-4830 in combination with KEYTRUDA in patients with advanced solid tumors. Expansion cohorts of this study include pancreatic adenocarcinoma, glioblastoma, head and neck squamous cell carcinoma (recurrent or metastatic; PD-L1 positive), advanced NSCLC and gastric cancer.
MK-6482 (HIF-2α Inhibitor): Results in VHL-Associated RCC and Non-RCC Tumors (Abstract #LBA26)
In this Phase 2, open-label, single-arm trial, MK-6482 was evaluated for the treatment of VHL-associated RCC (NCT03401788). New data include findings for MK-6482 in VHL patients with non-RCC tumors and updated data in VHL patients with RCC. First-time data in VHL-associated RCC were presented in the virtual scientific program of the 2020 American Society of Clinical Oncology (ASCO) Annual Meeting. The study enrolled adult patients with a pathogenic germline VHL variation, measurable localized or non-metastatic RCC, no prior systemic anti-cancer therapy, and Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0 or 1. Patients received MK-6482 120 mg orally once daily until disease progression, unacceptable toxicity, or investigator’s or patient’s decision to withdraw. The primary endpoint was ORR of VHL-associated RCC tumors per RECIST v1.1 by independent radiology review. Secondary endpoints included DOR, time to response, PFS, efficacy in non-RCC tumors, and safety and tolerability.
Promising clinical activity continues to be observed with MK-6482 in treatment-naïve patients with VHL-associated RCC. Among 61 patients, results showed a confirmed ORR of 36.1% (95% CI, 24.2-49.4); all responses were partial responses, and 38% of patients had stable disease. The median time to response was 31.1 weeks (range, 11.9 to 62.3), and median DOR was not yet reached (range, 11.9 to 62.3 weeks). Additionally, 91.8% (n=56) of patients had a decrease in size of target lesions. Median PFS has not been reached, and the PFS rate at 52 weeks was 98.3%. Median duration of treatment was 68.7 weeks (range, 18.3 to 104.7), and 91.8% of patients were still on therapy after a minimum follow-up of 60 weeks.
In patients with non-RCC tumors, results in those with pancreatic lesions (n=61) showed a confirmed ORR of 63.9% (95% CI, 50.6-75.8), with four complete responses and 35 partial responses. Additionally, 34.4% had stable disease. In those with central nervous system (CNS) hemangioblastoma (n=43), results showed a confirmed ORR of 30.2% (95% CI, 17.2-46.1), with five complete responses and eight partial responses. Additionally, 65.1% had stable disease. In patients with retinal lesions (n=16), 93.8% of patients had improved or stable response.
In this Phase 2 study, TRAEs occurred in 98.4% of patients, and there were no Grade 4-5 TRAEs. The most common all-cause adverse events (≥20%) were anemia (90.2%), fatigue (60.7%), headache (37.7%), dizziness (36.1%) and nausea (31.1%). Grade 3 all-cause adverse events included anemia (6.6%), fatigue (4.9%) and dyspnea (1.6%). One patient discontinued treatment due to a TRAE (Grade 1 dizziness).
As announced, data spanning more than 15 types of cancer will be presented from Merck’s broad oncology portfolio and investigational pipeline at the congress. A compendium of presentations and posters of Merck-led studies is available here. Follow Merck on Twitter via @Merck and keep up to date with ESMO news and updates by using the hashtag #ESMO20.
About Vibostolimab
Vibostolimab is an anti-TIGIT therapy discovered and developed by Merck. Vibostolimab binds to TIGIT and blocks the interaction between TIGIT and its ligands (CD112 and CD155), thereby activating T lymphocytes which help to destroy tumor cells. The effect of combining KEYTRUDA with vibostolimab – blocking both the TIGIT and PD-1 pathways simultaneously – is currently being evaluated across multiple solid tumors, including NSCLC and melanoma.
About MK-4830
MK-4830 is a novel antibody directed against the inhibitory immune checkpoint receptor immunoglobulin-like transcript 4 (ILT4). Unlike current T cell-targeted antibodies (e.g., anti-PD1, anti-CTLA-4), anti-ILT4 is believed to attenuate immunosuppression imposed by tolerogenic myeloid cells in the tumor microenvironment. MK-4830 is currently being evaluated alone and in combination with KEYTRUDA across multiple solid tumors as part of ongoing Phase 1 and 2 trials.
About MK-6482
MK-6482 is an investigational, novel, potent, selective, oral HIF-2α inhibitor that is currently being evaluated in a Phase 3 trial in advanced RCC (NCT04195750), a Phase 2 trial in VHL-associated RCC (NCT03401788), and a Phase 1/2 dose-escalation and dose-expansion trial in advanced solid tumors, including advanced RCC (NCT02974738). Proteins known as hypoxia-inducible factors, including HIF-2α, can accumulate in patients when VHL, a tumor-suppressor protein, is inactivated. The accumulation of HIF-2α can lead to the formation of both benign and malignant tumors. This inactivation of VHL has been observed in more than 90% of RCC tumors. Research into VHL biology that led to the discovery of HIF-2α was awarded the Nobel Prize in Physiology or Medicine in 2019.
About KEYTRUDA® (pembrolizumab) Injection, 100 mg
KEYTRUDA is an anti-PD-1 therapy that works by increasing the ability of the body’s immune system to help detect and fight tumor cells. KEYTRUDA is a humanized monoclonal antibody that blocks the interaction between PD-1 and its ligands, PD-L1 and PD-L2, thereby activating T lymphocytes which may affect both tumor cells and healthy cells.
Merck has the industry’s largest immuno-oncology clinical research program. There are currently more than 1,200 trials studying KEYTRUDA across a wide variety of cancers and treatment settings. The KEYTRUDA clinical program seeks to understand the role of KEYTRUDA across cancers and the factors that may predict a patient’s likelihood of benefitting from treatment with KEYTRUDA, including exploring several different biomarkers.
Selected KEYTRUDA® (pembrolizumab) Indications
Melanoma
KEYTRUDA is indicated for the treatment of patients with unresectable or metastatic melanoma.
KEYTRUDA is indicated for the adjuvant treatment of patients with melanoma with involvement of lymph node(s) following complete resection.
Non-Small Cell Lung Cancer
KEYTRUDA, in combination with pemetrexed and platinum chemotherapy, is indicated for the first-line treatment of patients with metastatic nonsquamous non-small cell lung cancer (NSCLC), with no EGFR or ALK genomic tumor aberrations.
KEYTRUDA, in combination with carboplatin and either paclitaxel or paclitaxel protein-bound, is indicated for the first-line treatment of patients with metastatic squamous NSCLC.
KEYTRUDA, as a single agent, is indicated for the first-line treatment of patients with NSCLC expressing PD-L1 [tumor proportion score (TPS) ≥1%] as determined by an FDA-approved test, with no EGFR or ALK genomic tumor aberrations, and is stage III where patients are not candidates for surgical resection or definitive chemoradiation, or metastatic.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with metastatic NSCLC whose tumors express PD-L1 (TPS ≥1%) as determined by an FDA-approved test, with disease progression on or after platinum-containing chemotherapy. Patients with EGFR or ALK genomic tumor aberrations should have disease progression on FDA-approved therapy for these aberrations prior to receiving KEYTRUDA.
Small Cell Lung Cancer
KEYTRUDA is indicated for the treatment of patients with metastatic small cell lung cancer (SCLC) with disease progression on or after platinum-based chemotherapy and at least 1 other prior line of therapy. This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
Head and Neck Squamous Cell Cancer
KEYTRUDA, in combination with platinum and fluorouracil (FU), is indicated for the first-line treatment of patients with metastatic or with unresectable, recurrent head and neck squamous cell carcinoma (HNSCC).
KEYTRUDA, as a single agent, is indicated for the first-line treatment of patients with metastatic or with unresectable, recurrent HNSCC whose tumors express PD-L1 [combined positive score (CPS) ≥1] as determined by an FDA-approved test.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with recurrent or metastatic head and neck squamous cell carcinoma (HNSCC) with disease progression on or after platinum-containing chemotherapy.
Classical Hodgkin Lymphoma
KEYTRUDA is indicated for the treatment of adult and pediatric patients with refractory classical Hodgkin lymphoma (cHL), or who have relapsed after 3 or more prior lines of therapy. This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials.
Primary Mediastinal Large B-Cell Lymphoma
KEYTRUDA is indicated for the treatment of adult and pediatric patients with refractory primary mediastinal large B-cell lymphoma (PMBCL), or who have relapsed after 2 or more prior lines of therapy. This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials. KEYTRUDA is not recommended for treatment of patients with PMBCL who require urgent cytoreductive therapy.
Urothelial Carcinoma
KEYTRUDA is indicated for the treatment of patients with locally advanced or metastatic urothelial carcinoma (mUC) who are not eligible for cisplatin-containing chemotherapy and whose tumors express PD-L1 [combined positive score (CPS) ≥10], as determined by an FDA-approved test, or in patients who are not eligible for any platinum-containing chemotherapy regardless of PD-L1 status. This indication is approved under accelerated approval based on tumor response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
KEYTRUDA is indicated for the treatment of patients with locally advanced or metastatic urothelial carcinoma (mUC) who have disease progression during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
KEYTRUDA is indicated for the treatment of patients with Bacillus Calmette-Guerin (BCG)-unresponsive, high-risk, non-muscle invasive bladder cancer (NMIBC) with carcinoma in situ (CIS) with or without papillary tumors who are ineligible for or have elected not to undergo cystectomy.
Microsatellite Instability-High or Mismatch Repair Deficient Cancer
KEYTRUDA is indicated for the treatment of adult and pediatric patients with unresectable or metastatic microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR)
This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials. The safety and effectiveness of KEYTRUDA in pediatric patients with MSI-H central nervous system cancers have not been established.
Microsatellite Instability-High or Mismatch Repair Deficient Colorectal Cancer
KEYTRUDA is indicated for the first-line treatment of patients with unresectable or metastatic MSI-H or dMMR colorectal cancer (CRC).
Gastric Cancer
KEYTRUDA is indicated for the treatment of patients with recurrent locally advanced or metastatic gastric or gastroesophageal junction (GEJ) adenocarcinoma whose tumors express PD-L1 (CPS ≥1) as determined by an FDA-approved test, with disease progression on or after two or more prior lines of therapy including fluoropyrimidine- and platinum-containing chemotherapy and if appropriate, HER2/neu-targeted therapy. This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials.
Esophageal Cancer
KEYTRUDA is indicated for the treatment of patients with recurrent locally advanced or metastatic squamous cell carcinoma of the esophagus whose tumors express PD-L1 (CPS ≥10) as determined by an FDA-approved test, with disease progression after one or more prior lines of systemic therapy.
Cervical Cancer
KEYTRUDA is indicated for the treatment of patients with recurrent or metastatic cervical cancer with disease progression on or after chemotherapy whose tumors express PD-L1 (CPS ≥1) as determined by an FDA-approved test. This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials.
Hepatocellular Carcinoma
KEYTRUDA is indicated for the treatment of patients with hepatocellular carcinoma (HCC) who have been previously treated with sorafenib. This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials.
Merkel Cell Carcinoma
KEYTRUDA is indicated for the treatment of adult and pediatric patients with recurrent locally advanced or metastatic Merkel cell carcinoma (MCC). This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials.
Renal Cell Carcinoma
KEYTRUDA, in combination with axitinib, is indicated for the first-line treatment of patients with advanced renal cell carcinoma (RCC).
Tumor Mutational Burden-High
KEYTRUDA is indicated for the treatment of adult and pediatric patients with unresectable or metastatic tumor mutational burden-high (TMB-H) [≥10 mutations/megabase (mut/Mb)] solid tumors, as determined by an FDA-approved test, that have progressed following prior treatment and who have no satisfactory alternative treatment options. This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials.
Contacts
Media Contacts:
Pamela Eisele
(267) 305-3558
Justine Moore
(908) 740-6449
Investor Contacts:
Peter Dannenbaum
(908) 740-1037
Courtney Ronaldo
(908) 740-6132

In emotional displays, thousands honored Justice Ginsburg and vowed to protect her legacy. President Trump said the nominee “will be a woman,” and pressed to fill the seat “without delay.”

— NYT

The news media landscape has been evolving, where independent bloggers and freelancers are an essential part of the news ecosystem, which supports our democracy. 
Nevertheless, due to the new digital era and the independent roles that have been established, some bloggers and journalists are experiencing revenue disadvantages in funding for small blog businesses, and from advertisement networks such as Google AdSense.
They lack diversity, equity and inclusion (DEI).
An example of the changes in the journalism industry exists even with the New York Times that has transitioned from a traditional newsroom with a large daily newspaper circulation, to include a robust digital online presence nowadays. Many other publications these days do not even have print copies but are now only online.
With emerging online news options, the entire business at large continues to change. Headlines and news leads no longer strictly adhere to traditional Associated Press (AP) rules, in terms of length and forbidden English articles such as “the,” “a” and “an.” The game is so different now because the Internet provides unlimited space for content.
But with so much in and a lot more gone from our newsrooms, who will be paying for the new technology and those using it for freelance and independent work?
Is the answer the collaboratives such as The Lenfest Institute and Facebook Journalism Project?
“The Lenfest Institute team was hired in Sept. 2016, and our first major grant program was 2017,’’ stated Jim Friedlich, who is part of the Lenfest-FJP team.
Many other organizations such as grant funders for Journalism projects and initiatives are on the rise to endeavor in assisting with business costs and revenues. But who gets these funds? Do all eligible and qualified journalists get their fair share? The answer is, NO!
The Google News Initiative, for example, tries to be inclusive with each of their different funding projects. 
“We try to fund for a diversity of applicants, so we change the themes, too: From local and technology to diversity equity and inclusion,” explained Madhav Chinnappa, director of News Ecosystem Development at GNI.
The GNI has been funding innovative Journalism projects for a few years now, and since the COVID-19 Pandemic, it even funded journalists just to help with emergency revenues. But still, the DEI efforts to fund all eligible applicants have not been fully successful.
This is where we experience the adverse effects of traditional journalism out, and digital in. With all the newspaper industry changes and the issues of downsizing, the Internet has replaced a lot of manpower, or people needed for newsroom jobs.
So, now we have social media, bloggers, and independent Journalists doing the traditional newsroom jobs that must go on in a digital era. This is a big deal. Everyone now has a stronger voice. Democracy is very much alive. But not everyone is getting paid.
Journalist are still carrying on the voice of their local newspapers in a digital way. The problem is, who pays the digital journalists now? How do bloggers and Independent Journalist get paid for helping to keep our democracy functioning?
There are a few true and tried methods for revenue: Of course, the grant funders make an effort; also do the advertisement networks such as Google AdSense and others, and thanks to readers’ contributions.
But all that is not enough when some independent journalists are constantly working and posting their stories but are not making a living wage. It seems this disparity affects minorities because of the built-in systematic injustices that are tied into the new journalism revenue systems.
Grant funding is never guaranteed even though minority applicants are very eligible and over-qualified. Neither are the payments from Google AdSense diverse, equitable or inclusive. Minority journalists always have to compete for a paycheck. This is a huge discrepancy in the revenue system and for our shared democracy.
Although Chinnappa states that Google Adsense does not intentionally lack DEI, and “that it is definitely not the intent in any of (Google) products,” to show disparity, some Journalist are just not happy with the current revenue system that significantly limits payments for those who work, but are not as accepted or as popular.
Our democracy needs all our voices, not just some. That’s why voting matters for all, and so does journalism.
Now, with everyone having a place online to speak up and help to contribute to a variety of discourses, communities have a greater sense of our common humanity, and a better understanding of who we all are, and our place and purpose in society.
All people matter. All of our voices and our purposes matter.